Podcast
Youtube
Dr. Okoroha: So, I thought our first topic we would talk about is the current thinking of hip preservation, from hip arthroscopy, PAO to total hip arthroplasty. Rafa what are the causes of hip dysplasia and how do patients usually present?
Dr. Sierra: That's a great question, so I mean there's really only one cause and it's at birth. This is usually a condition that when we're seeing them it's because the patient has had untreated hip dysplasia meaning that at birth it was never caught or they may have had treatment for hip dysplasia usually with non-surgical treatments such as Pavlik harnesses, which are braces or even casting at childhood and they may have some residual hip dysplasia that needs to be treated. It's very interesting, so it's commonly seen in firstborn woman, that's probably the most common patient that I see sometimes associated with breach position. But it can occur really in any child in any family but most commonly it's in the oldest female patient
Dr. Okoroha: How do these patients usually present to your clinic?
Dr. Sierra: Most patients present with hip pain and it's important to note that the hip really doesn't hurt where most people think it hurts up towards the iliac crest or in the hip bone, these patients usually present with hip pain which they describe as pain in the groin. That's the most common location of their pain and it can also be associated with what we call mechanical symptoms, which is catching or locking in the hip. There's some patients that may present with symptoms of giving way in the hip joint or instability but that is less common or with symptoms associated with hip weakness and they may have pain towards the outside part of the hip mainly because the muscles on the outside part of the hip can get fatigued with extreme activities or uses. Although the majority of patients present with groin pain there's a subset of patients that may present with other areas around the hip that are painful as well.
Dr. Okoroha: Once they present to your clinic you've done the exam, what image modalities are you currently using to work up patients with hip dysplasia?
Dr. Sierra: Our standard imaging modalities for all patients that are young that are coming in with what seems to be hip related symptoms we get standard radiographs including an AP of the pelvis, we get a lateral hip x-ray usually a frog leg lateral. Then we get a Dunn view and there are different views that you can get called Dunn but the 45 Dunn view is the most common x-ray that we get. That's just a special x-ray to look specifically at the neck of the femur and it's anterolateral, then another one in the anterior aspect of the neck to see if they could have concomitant femoral deformities that could also be associated with hip dysplasia as well as other causes of hip pain such as impingement.
Dr. Okoroha: We know there's certainly different radiographic parameters that you look for that tell you how much dysplasia vs impingement. How often are you getting advanced imaging for a patient with displays? Are you getting an MRI or a CT routinely or can you tell everything you need to know on the x-ray?
Dr. Sierra: An MRI has become the standard of practice mainly because the majority of these patients will present with labral pathology. The labrum is a structure that deepens the socket and in some patients with instability they could have tears in the labrum and so the MR has become pretty much the standard of care for these patients. What is controversial is whether you should have contrast in the hip joint or not. The majority of patients that I see already have an MRI by the time I see them. A CT scan is an option for some patients that have both socket-sided problems as well as potentially some femoral sided issues either a large femoral neck deformity or what we call a CAM lesion or in certain circumstances patients may present with abnormal femoral version and that could be described better as like the twist that the femur has. They have an abnormal twist either towards the front or towards the back and these patients should be evaluated with a CT scan so you can get a sense of what the combined version or combined twisting of both the femur and socket is so that you can make a decision preoperatively as to whether they need additional surgery other than our standard of care.
Dr. Okoroha: So once you get your imaging, you've got your exam, what are your indications for surgery in a patient with hip dysplasia?
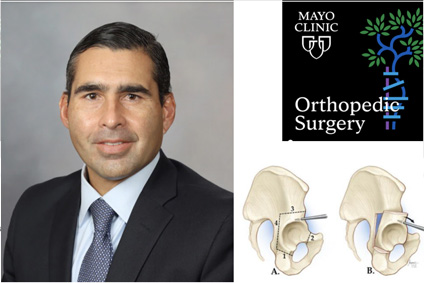
Dr. Sierra: By the time I see patients and to tell the truth the diagnosis of this condition has become more commonly diagnosed by practitioners and by multiple practitioners I mean primary physicians are now getting x-rays and being able to diagnosis a little bit easier. Our sports medicine colleagues are also making this diagnosis and so by the time they reach me it's because they've already had the diagnosis of hip dysplasia and many patients have already undergone appropriate non-operative management which is the first step and the first step of non-operative management is limitation of their activities because many of them have pain that is activity related and usually activities of high level or high impact activities. Many of these patients are gymnasts or hurdlers or soccer players. And so stopping their activities and seeing how they respond to that is important. Physical therapy especially if they have weakness or any pain with muscle fatigue is important and see how they do. I would say that probably 90 percent of patients respond to that temporarily. Unfortunately many of them if they truly have a dysplastic hip once they start to engage back into their activities will start having pain again and those are the patients that then if they clearly have dysplasia and that is that the femoral head is uncovered by the socket and has all the radiographic features associated with hip dysplasia then those patients are good candidates for a procedure that we call a periacetabular osteotomy. Which is a an osteotomy or a procedure that we do around the hip bone or the pelvic bone to turn the socket around so that we can improve the coverage of the femoral head. It's what we call a reorientation osteotomy of the hip and this is a fascinating procedure that's been around for three decades now or more and has shown excellent results for these patient
Dr. Okoroha: That's great and we know that you're one of the experts in the field and perform that surgery fairly often. What are the current outcomes with the PAO procedure?
Dr. Sierra: That's a great another great question because the way that I look at this is that there are really three objectives with the procedure. The first objective to me is to manage the patient's pain that they have, now and that means many of these patients present and we've written papers with the ANCHOR group showing that these patients that present prior to periacetabular osteotomy have significantly decreased patient reported outcome forms compared to matched controls so clearly these patients are not doing well from patient functional standpoint. So the first objective of the PAO is to help them with that and we've written several papers now showing that we're able to increase those patient report outcome scores at a year or two even past what we call the MCID (minimally clinical important difference)
which is a measure that we use to see how well we've done. And if we've met that MCID that means that these patients are doing much better than pre-operatively. So that's objective number one, objective number two is to get them back to their previous activity meaning sporting activities or activities of daily living and that's a different situation because although many patients are improved with their activities of daily living we've looked at the results of getting back to sporting activities and about a year out it's about half of the patients. There are reasons why they can't I mean very few are actually related to the hip pain, they're more related to other reasons. “the doctor told me not to do it again”, number two “I was a hurdler in in college and i'm done with college so i'm not doing it again”, “i'd rather not do it”, but many of them are able to get back to certain level of activities but only half of patients at a year are able to get back to high level athletic activities. Although i've had plenty of patients that have been able to get back to running marathons triathlons and play competitive sports again, but if you look at all comers then that's about half of people at about a year. We still have to look at it a little bit further out but at a year that's what's going on. So that's important from an expectation standpoint, that's really important to discuss with your patients because it is a big operation and the third objective is really the whole what I call the holy grail, is to really change the natural history of this hip. So we know that these patients if untreated will carry a risk down the road of developing arthritis in their hip joint and the third objective we've been able to meet by decreasing that risk about 50 percent at 10 and 20 years.so the results are overall overwhelmingly positive for these patients.
Dr. Okoroha: That sounds like pretty reasonable results especially with what they're predisposed to without surgery. We know that some patients have borderline hip dysplasia and they might have a little bit of femoroacetabular impingement as well and in those patients how are you deciding between hip arthroscopy versus a PAO? Are you doing a combination? How do you make that decision?
Dr. Sierra: What we're talking about is a patient that has borderline coverage of the femoral head, may have what we call a lateral center of angle between 18 or 25 degrees. So there are two patients that present this way there's a true dysplastic hip that has borderline coverage and those that patient will present with symptoms that are more instability symptoms and their range of motion is usually pretty normal or even increased. They may have increased acetabular or femoral version as well while the other patient is usually a male patient that has even decreased range of motion in their hip with then borderline acetabular coverage. I do think that patients present more with impingement type symptoms and they may have a CAM deformity or a femoral head and neck junction abnormality. So those are two different patients and they both could be treated with the Periacetabular osteotomy. It would be more likely on the patient with the symptoms of impingement to respond to an arthroscopic procedure as well but then ignoring the abnormal load through the acetabulum may or may not catch up to them down the road even though you may have improvements in the acute symptoms at this time. So I have a thorough discussion with the patients that many of these patients with impingement symptoms alone may have improvements in the symptoms now and it's really getting a sense for what they're willing to accept down the road because we do know even in in our natural history study that the patients that did the worst were that specific group that had impingement as well as mildly dysplastic hips. I think that there is a reason for that, if you think about the what happens with long-term impingement of the hip there's eventual damage to the socket with continued impingement and if you already have a small roof and you impinge into that and you damage it well that makes the roof even more narrow and so those patients will have the rapid progression. Those are the patients that I typically see with less than 40 years of age with pretty severe arthritis requiring a total hip replacement. After a thorough discussion with the patient if they feel that they want to treat a condition that could have a poor prognosis down the road then I would recommend doing both procedures at the same time. Sometimes we stage the procedures but sometimes we do it in the same setting but at least within a reasonable time frame and that would entail sometimes going in arthroscopically repairing the labrum treating the cartilage damage doing a femoral head neck junction osteochondroplasty and then in a subsequent procedure which is usually staged no later than a month afterwards we would do the PAO to improve the coverage of the femoral head.The tricky part about these patients is that they already have poor range of motion and then you do the pao they will lose a little bit more range of motion with the correction of the socket so you have to be very careful as to not over correct them otherwise they'll impinge even more and some of these patients that have combined dysplasia and CAM and femoral retrotorsion we've even gone even towards the extremes where we've actually done femoral anteverting osteotomies or de-rotational osteotomies to help improve that range of motion before impingement.
Dr. Okoroha: Okay great and so you touched on a certain subset of patients, the young patients with advanced arthritic change. Maybe they had dysplasia that was under treated, I see these patients often. What are your indications for a hip replacement in those young patients versus trying some alternative treatments?
Dr. Sierra: If the patient is young we certainly try to avoid a hip replacement as long as possible. The problem is that many young patients are really debilitated with their condition, we're not even talking about sports anymore we're talking about getting up sitting just hanging out. They're gaining weight they're mad because they can't exercise they're now only doing you know minor activities such as an elliptical and biking and they still have pain. I mean these patients unfortunately are at point and what I do feel is that if you have a dysplastic hip and you have a short segment of roof and now that becomes damaged that's even worse now so those patients tolerate much less arthritic changes than the patients that have normal joints. So those patients usually end up having to have the hip replacement at a very young age and although we usually tell them that they should wait as long as they can I mean many of these patients with dysplasia will need a hip replacement at fairly young age and will try non-operative things. Of course we'll try injections we'll try some with cortisone I mean there are other types of injections that are done by our sports medicine colleagues that have provided some relief but they all are short-lived. I mean we're just trying to buy some time before their hip replacement when we're talking about the long-term durability of these joint replacements we also have to take into account the problems that could occur with delaying joint replacement. I tell patients there's no difference if you're 33 or 34 if you could wait five years and be 38 who knows what we'll do in five years from now or more importantly we're gonna learn five years of what we've been doing now. So if you can wait five or ten years it's great go ahead and wait and many people say yeah i'm doing okay I know what I have and i'll be happy to wait because I can. Other people say I can't wait i'm ready to have the hip replaced and it doesn't matter that i'm 33 or they're 33 and a half that we're talking about longevity in decades of the hip replacement today and I don't think it makes much difference.
Dr. Okoroha: Great points Rafa. I've been taking some notes here, i'm going to try to summarize. We first talked about hip dysplasia and it's usually caused from a birth abnormality or untreated hip dysplasia, usually in that first female born patient and they're going to present with hip pain in the groin but it can be associated with some mechanical symptoms or some instability. You said the standard imaging includes x-rays but MRIs’ have become standard of care due to soft tissue abnormalities. CT scans are an option for socket or femoral sided problems as well. Your indications for PAO are failure of conservative management and radiographic indicators of hip dysplasia. You said the PAO outcomes are pretty good in decreasing pain and getting patients back to function and then lastly we talked about that young patient with advanced arthritic change and you said that they may be candidates for hip replacement especially if they become debilitated and conservative management fails.
Dr. Sierra: The only thing to add would be because we get that question all the time is okay i'm diagnosed with hip dysplasia but I have no pain, what to do then? and I think that my answer to that has always been I can't make you any better than no pain. So there's only one way that I can gauge the success of my surgery and it's with pain relief. So the worst thing that I could happen and i've seen is a patient with no pain undergoing a PAO and then coming back because now they have pain, so they're unhappy and they don't know why they underwent that big operation that's made them worse than what they were. So observation is fine keeping an eye on things, education is critical for all these conditions. Some people will accept what they have as long as they know why their hip hurts. “oh yeah okay I understand that now so I won't do this or do that, i'll change my lifestyle” and some people are willing to do it.
Dr. Okoroha: Ok so definitely not doing it in a preventative fashion so if somebody has abnormalities and no pain they don't need surgery. Great well thank you for taking time out to talk with us today
Dr. Sierra: No problem thank you for the invitation.