Sports medicine surgeon and team physician for the Minnesota Timberwolves Dr. Kelechi Okoroha joins host Dr. Jonathan Barlow to discuss modern thinking about hip impingement, an area of sports medicine that has undergone a rapid evolution over the last few years. Dr. Okoroha pays specific attention to indications, techniques, and the surgical learning curve.
Podcast
Youtube
Hip Impingement and Arthroscopy Podcast Transcript - Q & A
What is the current thinking about hip impingement? Is it congenital, is it developmental, where does it come from and how does it fit into hip pain in young athletes?
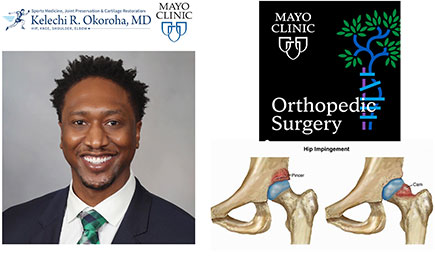
The understanding of hip impingement has expanded quite a bit over the last 10 years. We know that hip impingement is defined as abnormal contact between the femoral head and acetabulum and that continues to be diagnosed at increasing rates over time. As we learn more about hip impingement our treatment algorithms continue to evolve. We first began with performing hip arthroscopies with isolated labral debridements. Then after we understood the importance of correcting the bony abnormalities and preserving the labrum surgeons started performing osseous corrections and labral repairs. Initially capsular closure was thought to be not so important, but I think the current literature really demonstrates that patients who undergo hip arthroscopy without capsular closure have decreased outcomes. So, I think it's important to perform capsular closure whenever possible. Currently we have evolved with surgical treatment to perform a comprehensive management of all the structures and that includes a labral repair, femoral neck osteochondroplasty, acetabuloplasty and then capsular closure whenever possible.
Is this process thought to be congenital, developmental, or some combination of the two? How are these bony abnormalities forming?
I like to put the hips at risk of impingement into three categories:
- You can have abnormal anatomy and normal use, which speaks to either congenital abnormalities such SCFE (slipped capital femoral epiphysis) and hip dysplasia or even prior surgery.
- You can have normal anatomy and abnormal use. This occurs when the use exceeds the tolerance of the joint structures. This can be an acute injury in a contact athlete or that can be a chronic injury involving either occupational or recreational use.
- The last category is a combination of abnormal anatomy and abnormal use which is really common as well.
Once femoroacetabular impingement (FAI) develops and patients continue to use their hips does this lead to arthritis in the future?
We do believe that hip impingement can lead to early arthritis. In fact research has demonstrated that anywhere from 70 to 90% of all hip arthritis cases are caused by either FAI or hip dysplasia .
What about middle-aged or slightly older patients with hip pain. How do you go about the work up and evaluate if they're a candidate for hip preservation or if they need to go down a different road, let's say toward total hip replacement?
The middle age population is the most difficult population to treat. The young athletic population is straight forward, they usually have an acute labral tear and a large CAM (femoral neck) deformity. But middle-aged patients are similar to the degenerative meniscus tears at times. If you image everyone over 40 and get a hip MRI you're going to find a lot of patients with labral tears and osseous deformities. The question is who needs treatment? In those sets of patients, it's important to exhaust your non-object management with physical therapy, NSAIDs, and injections to see who really needs surgery. We have done research to evaluate which patient factors lead to increased success after hip arthroscopy and a few of those factors are: lower BMI, younger age (especially under 45), decreased arthritis, and treatment within six months.
In younger more straight forward patients do you go through the process of physical therapy, MRI and an injection or is this situation where you say the anatomy is problematic enough that you proceed to surgery? How do you make that decision?
That is a great question because treatment differs based on age in certain situations. In younger patients are I still do a trial of physical therapy and obtain advanced imaging (MRI). However, in a young patient who’s history and exam are straightforward I don't require a steroid injection as there are risk associated with any procedure. In those cases, after they fail physical therapy I offer surgery to correct the pathology.
For the older patients, with mild arthritis with better patient characteristics, is there a role for hip arthroscopy? Or should patients just wait for hip replacement? How do you decide to finally indicate somebody for hip arthroscopy?
There's definitely a role in those ideal patients who are middle aged with lower BMI who do not have end stage arthritis. For those patients I usually do an injection for two reasons.
- It is diagnostic. If I perform an injection in the hip and that patient gets pain relief, I know definitively then that pain is coming from inside hip and not from the surrounding muscles or lower back.
- It gives them some therapeutic pain relief and allows them to really do physical therapy without much pain. This allows us to see if their symptoms can be treated non-operatively. In these patients that fail conservative management, I indicate them for a hip arthroscopy.
What are your thoughts about time frame after injection to surgical management? Do you have a cutoff that you like to go by?
Yes, usually no surgery for three months after a hip injection. I think the hip and knee literature is similar.
Can you talk a little bit more about the steps of the procedure? I know there are steps on the acetabular side and the femoral side. You talked about labral repair vs debridement and capsular closure. Do you do all of the procedures every time or is it individualized?
I try to treat patients in the a la carte manner based on the pathology present. If there is a labral tear, i try to preserve tissue and perform a labral repair whenever possible. Then I evaluate the femoral CAM deformity and the acetabular pincer deformity. Most patients have a combination of both, but I only treat the pathology present. If they have a cam deformity I perform a femoral osteochondroplasty to get the alpha angle under 55. If they have a pincer deformity with a large center edge angle, then I perform an acetabuloplasty. And all my patients get capsule closure.
Are these steps an intraoperative decision most of the time or is it more based on the radiographs and MRI scan?
For the most part you can see what is going on with the patient on an mri, however I do get ct scans on some of my patients, especially patients that I’m concerned have some version abnormality of the femur or the acetabulum. This allows you to assess that bony abnormality and be aware of what you will encounter surgically.
I have read about labral reconstruction as opposed to labral repair. What are your thoughts about that in the current age?
Labral reconstruction is a great tool to have. Those are going to be for the patients have a diminutive/degenerative labrum or have had previous procedures and don't have a lot of labrum left. Labral reconstruction is a procedure we can do where we take either an autograft or an allograft tissue and form a new labrum for that patient. This has started to be performed regularly over the last 10 years or so but we've done some recent research at RUSH evaluating an alternative procedure which is labral augmentation. Augmentation is a bit different in that you don't take down the whole labrum and put in new tissue. You really just augment the old labrum with new tissue placed directly on top of it. We know the labrum is an important hip stabilizer and provides a suction seal effect to the hip. Think about placing a suction cup on a glass, if you do a 360 degree resection around the edge and then fix it down in let’s say eight spots, in-between each fixation point is a potential space for air to escape if there is a problem with healing. Whereas with augmentation we put new tissue on top of the old tissue and there are less chances to lose that seal. Our early studies have shown improvements in establishing the hip suction seal with labral augmentation vs. reconstruction. Therefore, I am a fan of augmentation whenever possible.
Do you think there's a role for debridements in any patients or is that something that sort of has gone by the wayside?
Debridements are going to be more in older patients that have a degenerative labor tear with little tissue to repair. Those patients are still good candidates for debridement but for the most part we try to repair the labrum whenever we can.
Is the learning curve for hip arthroscopy fairly steep? My understanding is the costs are high if you don't get it quite right in terms of either cartilage defects or heaven forbid femoral neck fractures or other complications. Can you talk about some of the key components and maybe talk a little bit about the learning curve and thoughts about low volume hip arthroscopy surgeons?
Hip arthroscopy is not as common as shoulder or knee arthroscopy so it requires some additional expertise or training. For one it involves the use of a 70 degree scope which is more challenging, especially for residents and fellows to learn. Often fellows and residents do not get a lot of practice with hip arthroscopy in training. A key to a successful hip arthroscopy is performing the procedure in a traumatic nature, without damaging any cartilage or labrum while entering the hip or completing the surgery. This is not as easy to do without experience and therefore fellows and resident may not get as much practice. Hip arthroscopy is a surgery that needs a little bit more practice and detail in the lab and more familiarity with the 70 degree scope.
It sure sounds like with the complex indications and associated with the procedure, hip arthroscopies are best done by people who are doing a relatively high volume?
I’d agree it's best done by people that doing a high volume or hip arthroscopies. When we look at the most common reason for re-operation, we found it is inadequate bunny resection. So, you have to have experience in really resecting that cam to the proper level to avoid impingement. The second most common reason for reoperation is likely failed capsule closure or tear in the repaired capsule. We know that the iliofemoral ligament is the strongest ligament in the body and it is a key hip stabilizer of the hip. Early on with this surgery nobody used to repair the capsule, a lot of the times because it was too difficult. Now we're finding that those patients that didn't have capsule closure are doing worse than patients that do. So capsular closure is a key component of the procedure.
Can you talk about the technique around that capsular closure and then tie into that any emerging technologies that you see over the next few months or years that will come out which may dramatically change this game?
Capsule closure is dependent on the type of capsule incision. Some people make a straight incision in the capsule and some people perform a “T” in the capsule. What you want to do is make sure that you have a repair stich every one to two centimeters of capsule incision to make sure there is a tight repair.
There are a lot of emergent technologies that are current coming out. One can be used to map the bony deformities preoperatively and then you can correlate that intraoperatively to check the bony resection. These techniques are really useful, especially with surgeons that haven't done a lot of hip arthroscopies.
Any other thoughts that you'd like to add for people who are either interested in hip impingement or surgeons who want to maybe add it to their to their game or residents who are interested in it?
I would say if you are interested in hip arthroscopy make sure to go to a residency or fellowship that has somebody doing them in high volume, or make sure you to get a lot of practice in the lab. I don’t think people should be discouraged. I think if you want to perform hip arthroscopies there's plenty opportunities to get it done right.