Podcast
Youtube
Shoulder and Elbow: New technologies in shoulder arthroplasty Podcast Transcript
Host: [00:00:10] Welcome to the Mayo Clinic Orthopedic Surgery Podcast, a curated series of interviews and discussions highlighting the three shields of orthopedic surgery at Mayo Clinic, clinical practice, research and education.
Dr. Okoroha: Welcome to the mayo clinic ortho podcast. I am your host Dr. Kelechi Okoroha and we have the pleasure of having my esteemed colleague Dr. Joaquin Sanchez-Sotelo here with us today. Joaquin obtained his medical degree, PHD and orthopedic resident training at the autonomous university of Madrid. He then completed two adult reconstruction fellowships here at the Mayo clinic. Joaquin has an extensive research background and is well known for his work both here and internationally. He currently serves as the chief of our shoulder and elbow department here at the Mayo clinic. We are lucky to have Dr. Sanchez-Sotelo here with us to speak today. Welcome Joaquin.
Dr. Sanchez-Sotelo: Thank you very much Kelechi, thank you for the Opportunity.
Dr. Okoroha: How has 3d mapping or printing been incorporated into the realm of shoulder arthroplasty?
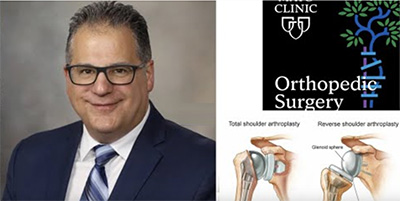
Dr. Sanchez-Sotelo: Well that is such a great question and it's interesting when I was in training as a resident and then on early my practice and we attempted to do a shoulder arthroplasty all we used to be honest was x-rays. Then we incorporated a CT scans and that was an eye opener because I don't think we fully understood the deformity of the shoulder especially for each patient and the features of bone loss and stability. So today as you very well know we get the CT scan of any patient that we're going to be operating on and we incorporate those into a software and there are many companies that provide software that is basically free of use. Then the software allows us to create a 3d rendering of the shoulder on a screen where you can rotate the models and you can get different measurements of version, inclination, subluxation, bone loss and then on top of that you can actually do your surgery and virtually place the implants wherever you want, wherever you think the patient will benefit the most from. So, it really has transformed into much more accurate surgery and also more personalized. So now we know where it is that we have to place our implants for each patient specifically based on their anatomy and deformity.
Dr. Okoroha: what is PSI or patient specific instrument and how does it improve our accuracy and outcomes when we're doing these surgeries?
Dr. Sanchez-Sotelo: Most shoulder surgeons use the acronym PSI for patient specific instrumentation and in the very basic form that means that once you have your plan with your software you can actually order a guide that is 3d printed and most of the times it is used for what we call the axis of most systems. When you're preparing the glenoid will base your preparation on a pin guide that is inserted and patient specific instrumentation allows you to place the pin exactly where you planned your surgery.
Dr. Okoroha: Is that also effective in getting your glenoid in the right position, because we know that's the most important part of the surgery?
Dr. Sanchez-Sotelo: That's exactly right, so it will tell you what's going to be the direction of your instruments that will basically end up preparing the glenoid so that you can match your version inclination and depth of reaming to what you planned before surgery.
Dr. Okoroha: How is navigation used in shoulder arthroplasty?
Dr. Sanchez-Sotelo: So navigation to be honest is still in its infancy. For the many people that may be listening, navigation essentially means that you get some instruments thatare called trackers and you place some in the anatomy. So, you're tracking the patient's anatomy the bones essentially you place some trackers in instruments and then the computer through cameras will recognize the relationship between the anatomy and the instruments and then real time as you modify your instrument you're going to see how the instrument rendering changes on the screen and allows you to target whatever angle you want or whatever direction you want. As of now there is only one company that is truly established in navigation and it's only for the glenoid so it's still starting and going well. But I think we're going to witness over this coming decade an explosion of navigation systems that are based on different things visual trackers mixed reality and eventually robotics.
Dr. Okoroha: Is the navigation that's in its infancy in the shoulder similar to what we've seen in the hip with total hips and total knees? And with robotics is that what we're seeing develop in the shoulder?
Dr. Sanchez-Sotelo: I think what we have seen in the lower extremities is that navigation was a first way to try to optimize the execution of a surgical plan. But if you go to meetings now or pay attention to what people are publishing we have gone one step further into robotics now there is a little bit of controversy there because some of the systems that people claim to be robotics are actually more sophisticated navigation without much robotics. But in general for hip and knee we're at a phase where robotics is being used or promoted widely whereas in the shoulder we're still at the navigation phase and again in its infancy.
Dr. Okoroha: : Do you see that as something in the future where we're using the similar robotics we have seen in the knee to get our glenoid position and shave off the bone on the glenoid as well?
Dr. Sanchez-Sotelo: No question, so I think robotics at least in my practice I hope it will be truly revolutionary because robotics is basically a way to prepare the bones exactly to what you desire based on your plans. So, the execution is perfect but it has a number of features that are very appealing to me. One of them is that robotic is very accurate within maybe less than a degree and maybe less than 0.1 millimeters. Number two it has this so-called haptic feedback that now we're used to it for example when you use an i-phone and you push on the screen for a long time it vibrates so it gives you feedback that is tactile, with a robot is the same thing you're preparing bone and if you go past what people call the boundaries, (which is what you don't want to go past because you will violate soft tissue) it will actually stop you. But the final thing is that you can prepare the bones with a very small instrument like a burr. As you know one of the limiting factors of arthroplasty today is that oftentimes you have to divide and then repair the subscapularis muscle tendon unit that needs protection, so patients are in a sling for four to six weeks. If we were able to prepare the bones of the shoulder through the interval region with a burr potentially you could do the whole operation through the interval region which means that you would be really soft tissue preserving and patients could remove the sling the day after surgery if they felt that their pain was controlled.
Dr. Okoroha: That's fantastic that sounds like some exciting things coming in the near future and so that's a little bit about robotics what about mixed reality. I know you've been really instrumental in developing mixed reality. Can you tell us about mixed reality and how you use it in your practice?
Dr. Sanchez-Sotelo: Robotics are coming but they're still a few years away I think so mixed reality is one way you can navigate the shoulder and the way that reality or mixed reality works is essentially by using a visor or a headset that will project into your eyes a combination of the real world and the virtual world. The system that I have helped design through mayo clinic and a company involves loading the pre-op planning in devices so that you can see real time in front of a patient what you're going to be doing in terms of your planning. But the next step will be to have markers like we use for classic navigation that can be recognized by these so-called hololens so then you can navigate through the visor and the hope is that one day you can do what we call markers-less navigation where you can look at the field and the hololens will recognize the changing shapes of the bones and without registration you can already start navigating. So i'm very excited about that technology that eventually will be surpassed by robotics or maybe it'll be used in different environments altogether.
Dr. Okoroha: How often are you looking at that mixed reality through their goggles and changing your plan or tweaking a little bit based on what you see through those visors?
Dr. Sanchez-Sotelo: I don't find myself changing the plan so much it's more that I can execute better the plan that I made. So mixed reality as of now I wouldn't think that you would use it to change your plans, more to look at the patient's anatomy without having to go back to a different screen. You see the plan projected and then you can basically copy in real time from the screen to what you're seeing in the patient and then as I said in the near future that will allow navigation as well.
Dr. Okoroha: [A lot of people are talking about 3d printing from instruments to implants to houses. How does 3d printing fit in the shoulder arthoplasty realm? Are there any times where we 3d print implants for the shoulder?
Dr. Sanchez-Sotelo: So that is coming as well and think very very quickly. So right now the interest is mostly in revision surgery so for those patients that there is so much bone missing especially on the glenoid that you and I know as surgeons that we couldn't really reconstruct the shoulder otherwise you can order a custom made 3d implant for revision. But very quickly we're going to see that in the setting of primary surgery as well. So i've heard that a couple of companies are working on 3d printed implants that are patient-matched for the deformities so you don't even have to ream the glenoid you can just clean a little bit any remaining cartilage or maybe bone irregularities and just it will just fit that patient perfectly. One thing that mayo has been a pioneer is in point-of-care 3d printing where we have a 3-printing lab in our facility as you know. The question there will be more regulatory does a hospital have enough documentation so that the FDA would allow printing implants in-house. So I think that will be more for compassionate use but there's no question that like with navigation robotics and mixed reality in the next decade we're going to see more and more implants that are printed for the patient.
Dr. Okoroha: Is that something you see coming into the near future here?
Dr. Sanchez-Sotelo: Yes, well I’m already using 3d printing implants for revision surgery pretty soon we'll be using them for some more complex primary surgery and maybe in the future for everyone .
Dr. Okoroha: Awesome so that's a lot of technology and development going on in the shoulder. Is there anything that we haven't touched on that you're getting into?
Dr. Sanchez-Sotelo: No, I just think that is really exciting to think that things that we apply today in our daily lives like I’m always amazed about how much we have evolved with different computers cell phones watches you know things that we can do to improve our quality life. In general I think medicine has lagged behind a little bit and partly because we have to make sure it is safe for our patients but now it's really exciting because we're going to see an explosion ultimately that I think is going to truly improve patient outcomes which is what you and I really like.
Dr. Okoroha: How often are patients coming to you asking you if can do robotic surgery or do you do 3d implants or patient specific instruments or are patients coming to you asking about that?
Dr. Sanchez-Sotelo: I get the question about robotics all the time and part of it is because as you know our knee replacement partners that may use robotic surgery and we share patients right so they come to me and say hey dr so-and-so did my knee with a robot can you do with the shoulder and I have to tell them unfortunately not yet but it's coming. But I started working on it but like I have all the things I can use so then I show them the pre op planning software, PSI, mixed reality and then the robot is almost here we're getting there.
Dr. Okoroha: I appreciate you taking your time to talk to us today i'm just going to summarize what you said here. You talked a little bit about 3d mapping you talked about how it allows us to get better detail and accuracy and shoulder arthroplasty. we talked about patient specific instruments which allow smaller instruments to be used. You talked a little bit about navigation, you said it's in its infancy but allows real-time tracking but it's mostly used for the glenoid. You also talked about robotics and how it's a structured way to prepare the bone accurately for replacements. Then we got into a little bit about mixed reality and it's a way to navigate the shoulder using a visor that combines the real world and the pre-operative plan and the way you can see it live on the patient. And then we talked about 3d printed implants, you're saying these are more used in revision shoulder arthroplasty and for patient specific implants. Anything else Joaquin?
Dr. Sanchez-Sotelo: No that's an excellent summary thank you for listening so carefully you're awesome.